July assessment gm
July assessment
Q1
1.PULMONOLOGY
2.NEUROLOGY
3.CARDIOLOGY
5.Infectious diseases (Mucormycosis, ophthalmology, Otorhinolaryngology)
6.GASTROENTEROLOGY
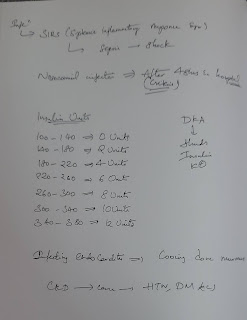
7.SEVERE COVID WITH DIABETES
8.INFECTIOUS DISEASE AND HEPATOLOGY
9.INFECTIOUS DISEASE( HI Virus, Mycobacteria, Gastroenterology, pulmonology )
10.CARDIOLOGY
Q2-4
Patient centered data around the theme of renal failure patients with AKI, CKD and acute on CKD,
captured by students from 2016 and 2019 batch in the links below
Patients with low back ache and renal failure
Q2) Share the link to your own case report of a patient that you connected with and engaged while capturing his her sequential life events before and after the illness and clinical and investigational images along with your discussion
https://siddarth43.blogspot.com/2021/07/aki-on-ckd.html?m=1
Q3) (Testing peer review competency of the examinees) :
Please go through the cases in the links shared above and provide your critical appraisal of the captured data in terms of completeness, correctness and ability to provide useful leads to analyze the diagnostic and therapeutic uncertainties around the cases shared.
AKI
https://laharikantoju.blogspot.com/2021/07/58-year-old-male-patient-elog-lahari.html?m=1
Over view
A 58 year old male patient came to casualty with chief complaints of-
lower abdominal pain 1 week
burning micturation 1week
low back ache after lifting weights
dribbling / decrease of urine out put 1week
fever 1 week
SOB , rest 1week
Apprisal
Case history was taken well and examination was very well done. Sequential evaluation of case is apprisiable
Negative points
It would be better if fever chart is added as it was treated with strict temp and IO monitoring as it would be better understood improvement of the case was not well mentioned
My Analysis
This is a case of Acute kidney injury( AKI) 2° to UTI, associated with Denovo - DM -2
With ? Right HEART FAILURE,With K/C/O - HTN ( Not on Rx)
-AKI causes a build-up of waste products in your blood and makes it hard for your kidneys to keep the right balance of fluid in your bodyand return of creatinine to the base line and symptoms less then 3 months indicating it to be a AKI
Acute on CKD :
http://srinaini25.blogspot.com/2021/07/srinaini-roll-no-33-3rd-semester-this.html
Over view
A 75yr old male patient ,labourer by occupation ,came to casuality with Cheif complaints of
Lower backache since 10days
dribbling of urine since 10days
Pedal edema since 3days
SOB at rest since 3days
Increased involuntary movements of both upper limbs since 10days .
Apprisal
I would not find any points to be highlighted . History was taken well
Negative points
There are no clinical pics of the symptoms like pedal edema.
Proper chronological order of symptoms apperance was not done
Fever chart was not included.
No IO charting was done though it was told it should be strictly monitored
My Analysis
This is case of
Acute renal failure (intrinsic)
Grade 1 L4-L5 Spondylodiscitis, Multifocal infectious Spondylodiscitis
Hyperuricemia 2° to Renal failure
Uraemia induced tremors( resolved)
Delerium 2° to septic /Uremic encephalopathy (resolving)
CKD :
https://krupalatha54.blogspot.com/2021/07/a-49-yr-old-female-with-generalized.html?m=1
Over view
A 49 yr old female , mother of 2 children, who is a house wife, apparently asymptomatic 13 yrs ago and then she noticed mass per anum with bleeding , went to hospital and diagnosed as haemorrhoids and got operated.
Since 3 yrs she has history of muscle aches, for which she is using NSAIDs.
She has h/o fever 20 days back, got treated in the local hospital, and
Since 20 days she has generalized weakness.
She also has h/o vomitings since 3 days, with food as content, non - projectile , non bilious.
Appraisal
History was taken well.
Good lab work clear evaluation was done
Negative points
There are no clinical pics of the symptoms like pedal edema.
Proper chronological order of symptoms apperance was not done
Fever chart was not included.
No IO charting was done though it was told it should be strictly monitoredit would have been better if urine was sent for eosinophils for interatial disease
My Analysis
This is case of CKD ?
Chronic interstitial nephritis secondary to plasma cell dyscariasis, (multiple myeloma - 70% plasmacytosis).
Patient with coma and renal failure
https://ananyapulikandala106.blogspot.com/2021/06/a-35yr-old-female-elog.html
Overview
A 35 yr old female with Fever and Diarrhea since 5 days( 4 to 5 times a day with blood discharge).
Back pain( 5 days ago) with abdominal pain and chest pain
appraisal
Very well presented
With good fever charting with all the necessary information.
History was taken detailed way
Follow up was good
All the tests were properly done
Negative
I could not find the negative data in the elog
Analysis
It could be the hypoxia which could have caused the permanent brain damage which was the reason for her vegetative state .
Subjectively she was told better but objectively no improvement was Seen. Hospitalisation has increased the infection to the bed sore it would have been better if discharged early as it was permanent damage and was impossible to treat anyway.
Q4: Testing scholarship competency of the examinees ( ability to read comprehend, analyze, reflect upon and discuss captured patient centered data as in their 'original' answers to the assignment for May 2021):
Please analyze the above linked patient data by first preparing a problem list for each patient (based on the shared data) and then discuss the diagnostic and therapeutic uncertainty around solving those problems. Also include the review of literature around sensitivity and specificity of the diagnostic interventions mentioned and same around efficacy of the therapeutic interventions mentioned for each patient.
Analysis the data
https://ananyapulikandala106.blogspot.com/2021/06/a-35yr-old-female-elog.html
Analysis of A 35 yr old female with Fever and Diarrhea since 5 days( 4 to 5 times a day with blood discharge).
Back pain( 5 days ago) with abdominal pain and chest pain
Vegetative state of the patient could be due to hypoxia which could have caused the permanent brain damage which was the reason for her vegetative state . Subjectively she was told better but objectively no improvement was Seen.
https://pubmed.ncbi.nlm.nih.gov/19362767/
Link supporting the data
Q 5) Testing scholarship competency in
logging reflective observations on your concrete experiences of this last month : (10 marks)
The elog /online learning from the hospital has been a new experience and we learnt quite lot of things through reflective observation during lockdown.
it's a bit challenging as we have just entered internship ,We have learnt elogging of the cases in a very short span of time and made juniors do so.
I could answer the questions from juniors easily as I have been part of many discussion in ICU and wards
Managing juniours has been a new experience challenging my managing skills.
By doing this assignment I could view many cases and many case scenarios through which I learned many things

Comments
Post a Comment